Sciatica is a common condition that affects millions of people in the United States, often causing pain, discomfort, and mobility issues that can significantly impact daily life. It refers to pain that radiates along the path of the sciatic nerve, which extends from the lower back down through the hips, buttocks, and legs. While sciatica can range in severity, understanding its causes, recognizing the symptoms, and exploring treatment options are essential for effective management and long-term relief.
What Is Sciatica?
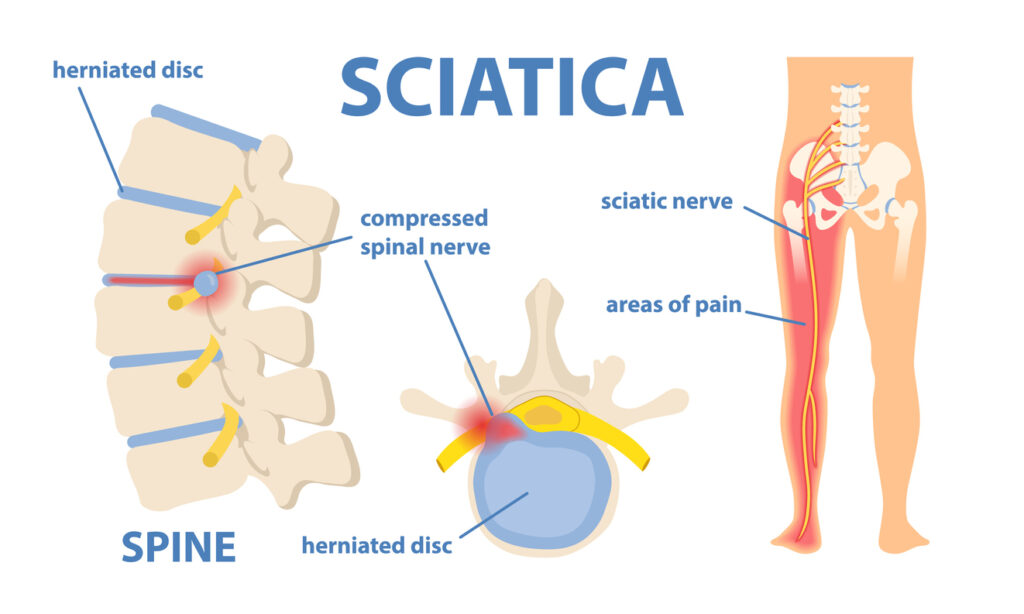
Sciatica is not a disease in itself but a symptom of an underlying medical condition that compresses or irritates the sciatic nerve. The sciatic nerve is the largest and longest nerve in the body, and when it becomes inflamed or pinched, it can result in sharp, burning, or shooting pain that travels down one side of the body. In many cases, the pain is accompanied by numbness, tingling, or muscle weakness in the affected leg.
Common Causes of Sciatica
The most frequent cause of sciatica is a herniated or slipped disc in the spine that presses on the sciatic nerve. Other potential causes include:
- Spinal stenosis: Narrowing of the spinal canal can put pressure on the nerve.
- Degenerative disc disease: Wear and tear of spinal discs with age can lead to nerve irritation.
- Spondylolisthesis: A condition where a vertebra slips out of place and compresses the nerve.
- Muscle spasms: Particularly in the piriformis muscle, which lies close to the sciatic nerve.
- Injury or trauma: Accidents or falls that impact the lower back.
- Tumors or infections (in rare cases): May also affect nerve function.
Obesity, a sedentary lifestyle, poor posture, and jobs that require heavy lifting or prolonged sitting can increase the risk of developing sciatica.
Recognizing the Symptoms
Sciatica symptoms can vary widely from person to person, but they commonly include:
- Pain that radiates from the lower back to the buttocks and down one leg
- Sharp or burning sensations
- Tingling or numbness in the leg or foot
- Muscle weakness or difficulty moving the leg or foot
- Pain that worsens when sitting, coughing, or sneezing
- A constant ache in the affected leg
The pain typically affects only one side of the body and can range from mild discomfort to severe and disabling.
Diagnosis and Medical Evaluation
To diagnose sciatica, healthcare providers will usually begin with a physical examination, taking note of symptoms and medical history. Tests may include:
- X-rays: To detect bone spurs or alignment issues.
- MRI or CT scans: To view soft tissue and determine if a herniated disc is present.
- Electromyography (EMG): To measure nerve and muscle activity and identify nerve damage.
Proper diagnosis is critical to ensure that the underlying cause of sciatica is treated effectively rather than just masking the symptoms.
Treatment Options for Sciatica
The majority of sciatica cases can be treated successfully with conservative measures. Here are the most common treatment approaches:
1. Physical Therapy
Physical therapy plays a central role in sciatica treatment. A trained therapist can develop a customized program to strengthen the muscles supporting your spine, improve flexibility, and promote better posture. Regular stretching and low-impact exercises, like walking or swimming, can also help relieve pressure on the sciatic nerve.
2. Medications
Over-the-counter pain relievers such as ibuprofen or acetaminophen can help reduce inflammation and pain. In some cases, doctors may prescribe:
- Muscle relaxants
- Anti-inflammatory drugs
- Nerve pain medications
- Corticosteroid injections (for more severe inflammation)
These should always be taken under medical supervision, especially when used long-term.
3. Heat and Ice Therapy
Applying ice packs to the affected area during the first few days can reduce inflammation. After that, heat therapy (like a heating pad or warm bath) can promote blood flow and aid healing.
4. Lifestyle Modifications
Small changes in daily habits can make a big difference. These may include:
- Avoiding prolonged sitting or standing
- Using proper lifting techniques
- Maintaining a healthy weight
- Sleeping on a supportive mattress
- Practicing good posture at work and at home
5. Alternative Therapies
Some individuals find relief through complementary approaches such as:
- Chiropractic care: Spinal adjustments may help relieve nerve pressure.
- Acupuncture: Can promote relaxation and reduce pain.
- Massage therapy: Helps relieve muscle tension that may be aggravating the nerve.
6. Surgical Intervention
Surgery is considered a last resort when other treatments fail to provide relief, or if there is significant nerve damage or loss of function. Common surgical options include:
- Microdiscectomy: Removal of a portion of the herniated disc that’s pressing on the nerve.
- Laminectomy: Removal of bone that’s compressing the nerve due to spinal stenosis.
Surgery can be effective, but it also carries risks, so it should be carefully discussed with a specialist.
